Prevention of retained surgical items
Surgical outcomes can be greatly impacted by errors in the OR. The hectic pace in the OR makes it an easy target for mistakes to happen. This section will cover the incidence of retained surgical items, the ramifications to patients, families and staff and evidence-based recommendations for prevention.
O.R. Safety Series: Retained Surgical Items
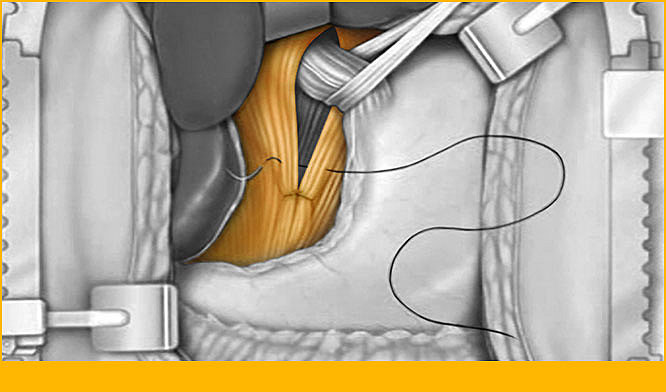
Every medical procedure comes with some risk to patient health. This is especially true for surgical procedures. Surgical items including instruments, sponges and sharps have been unintentionally left in body cavities after surgery. There are a myriad of reasons this could happen but regardless of the reason for the retention of an item, the patient will likely experience significant morbidity as well as pain and suffering. The best treatment is prevention.
This program will outline some of the factors that may lead up to retained items, as well as outline guidelines and technology for prevention.
Learning objectives
- Define retained surgical items (RSI)
- List the clinical, financial and legal implications of RSIs
- Review current practices for prevention of RSIs
- Discuss available practices and technology to prevent RSIs
Literature matters: Infected textiloma
Research bulletin: Infected textiloma, 35 years after the operation for femur fracture, an extremely rare occurance
Authors: Amir R. Sadeghifar, MD, Ali R. Saeed, MD
Literature matters: Which type of reaction in retained surgical sponges is more dangerous?
Research bulletin: What type of reaction in retained surgical sponges is more dangerous?
Authors: Mesut Gul, Ibrahim Aliosmanoglu, Burak Veli Ulger, Adbulla Oguz, Mehmet Guli
Literature matters: Supra-aural gossypiboma
Research bulletin: Case report of a retained textile surgical sponge in an unusal location
Authors: N. Chawla, N. Gupta, N. Dhawan
Using a data-matrix-coded sponge counting system across a surgical practice: impact after 18 months
Authors: Robert R. Cima, MD, MA, Anantha Kollengode, PhD, MBA, James Clark, RN, MS, Sarah Pool, RN, MS, Cheryl Weisbrod, RN, MS, Gwendolyn J. Amstutz, MHA, Claude Deschamps, MD
Retained surgical items (RSIs), most commonly sponges, are infrequent. Yet despite sponge-counting standards, failure to maintain an accurate count is a common error. To improve counting performance, technology solutions have been developed. A data-matrix-coded sponge (DMS) system was evaluated and implemented in a high-volume academic surgical practice at Mayo Clinic Rochester (MCR). The primary end point was prevention of sponge RSIs after 18 months.
The hidden costs of reconciling surgical sponge counts
Authors: Victoria M. Steelman, PhD, RN, CNOR, FAAN, Ann G. Schaapveld, BSN, RN, Yelena Perkhounkova, PhD, Hillary E. Storm, MSN, RN, CNOR, Michelle Mathias, BSN, RN
The purpose of this descriptive study was to estimate the cost of nonproductive OR time (ie. time spent not moving forward with the surgical procedure) required to reconcile surgical sponge counts and the time and costs of using radiography to rule out retained surgical sponges.
28996