Pressure injuries
It is important for caregivers to be knowledgeable about the intrinsic and extrinsic risk factors for the development of pressure injuries. It is also important to understand the basic causes of pressure injury: pressure, shear, friction and moisture. This section provides the latest evidence-based guidance on pressure injury risk, development, prevention and treatment strategies and tools for patient risk assessment.
Pressure injury prevention workshop
This course provides educational information for healthcare practitioners related to the physiology, etiology and prevalence of pressure injuries and reviews the latest evidence-based recommendations to prevention and treatment strategies.
Learning objectives
- Define a pressure injury
- List four risk factors associated with pressure injury development
- Describe pressure injury stages
- Name five pressure injury prevention interventions
- Describe pressure redistribution
Prevention is in: Reducing falls and saving skin in the ED
Learning objectives
- Understand statistics implicating ED origin of pressure injuries (PI) in the acute care setting
- Recognize characteristics of pressure injuries, including staging definitions and descriptions
- Understand the human and financial costs of pressure injuries
- Identify interventions useful for preventing pressure injuries in the ED environment
- Distinguish between the different types of falls
- Understand the human and financial cost of a fall
- Identify ED-specific risk factors for falls
- Identify evidence-based fall prevention practices in the emergency department
Heat, moisture, and the skin interface: the importance of microclimate management
Good clinical practice requires interventions geared toward minimizing the impact of pressure, shear, friction, and moisture on the patient’s skin. Each patient presents with unique challenges and risk factors that impact the care required. Many risk factors that impact the microclimate of the skin are uncontrollable (fever, perspiration, fluid loss); however, there are interventions that enable the caregiver to minimize the risk.
Pressure Injury Staging & Braden Scale Card
Pressure Ulcer Prevention Education Brochure
Tips to keep you safe!
What the experts say: Reduce the risk of heel pressure injury in the OR and the ICU
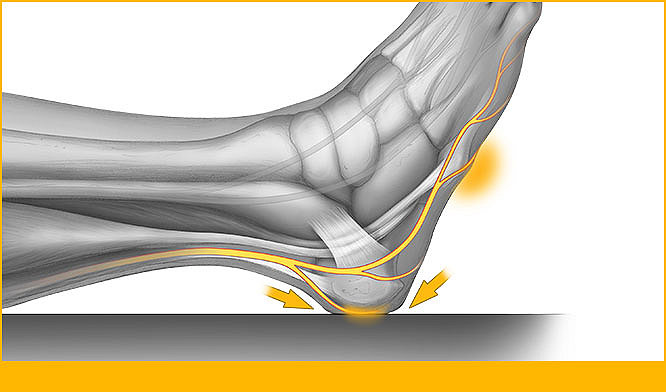
A pressure injury is localized damage to the skin and/or underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear.
What the experts say: Pressure injuries
A pressure injury is localized damage to the skin and/or underlying soft tissue, usually over a bony prominence or related to a medical or other device. The injury can present as intact skin or an open ulcer and may be painful. The injury occurs as a result of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, co-morbidities, and condition of the soft tissue.
What the experts say: Incontinence care and pressure injury prevention
Incontinence-Associated Dermatitis (IAD) is defined as “an inflammation of the skin that occurs when urine or stool comes into contact with perineal or perigenital skin.” IAD is also a major risk factor for pressure ulcers.
Quality Improvement Intervention with Patient Repositioning Device Results in HAPU Prevention and Cost Savings
Authors: Melinda Edger RN, BSN, CWOCN, Sheryl Bailey RN, BSN, CWOCN
A quality improvement initiative was designed using safe patient handling interventions to help prevent HAPUs in an intensive care unit (ICU).
The QI intervention was successful in preventing HAPUs, as demonstrated in Figure 2. Health care workers perceived the repositioning device required significantly less effort than standard of care. The improved HAPU outcomes resulted in significant cost savings and a documented return on investment (ROI).
A Comparative Study of Two Methods for Turning and Positioning and the Effect on Pressure Ulcer Development
Author: Jan Powers PhD, RN
Pressure Ulcers occur in 3 million people in the US. Patients must be effectively turned in order to relieve pressure that can result in skin breakdown. Multiple studies have demonstrated that appropriate turning does not get accomplished for patients as needed.
A blocked design with a convenience sample of 60 patients was used for this study. The comparison study was completed between standard of care (SOC) involving traditional turning using pillows and a new Turning and Positioning device (TAP).
A Successful Quality Improvement Initiative Results in Reduction of Hospital Acquired Heel and Sacral Pressure Ulcers
Author: Kathryn Bell MS, RN, CCRN, CCNS
Evidence-based HAPU prevention in the critically ill patient population requires adherence to best practices for prevention, and a focus on decreasing risk factors associated with HAPU development, such as moisture, friction, sheer, and prolonged pressure. A Quality Improvement initiative (QI) was designed to decrease sacral and heel HAPUs in critically ill patients.
Limited Mobility and the Foot: Plantar Flexion Contractures, Heel and Malleoli Pressure Ulcers, Peroneal Nerve Damage – How Can We Prevent Them? What Happens If We Don’t?
Author: Harriett B. Loehne PT, DPT, CWS, FACCWS
Prevention of facility-acquired pressure ulcers, plantar flexion contractures, and peroneal nerve compression is important. In order to do this, we must address calf compression, decreased circulation, hip external rotation, friction, shear, malnutrition, dehydration, moisture, positioning, exercise and early ambulation.
Risk assessments and guidelines are available for pressure ulcer prevention, which include many of these issues. Heel pressure ulcers and plantar flexion contracture risk can be decreased with a heel-offloading device, although use of such a device is contraindicated with existing fixed plantar flexion contractures and spasticity.
A literature search was performed to identify direct complications that arise from plantar flexion contractures. Except for indirect issues as PUs, falls, and potential complications from surgery, there were with minimal results in peer-reviewed literature. Many articles are available discussing prevention and control. Best practice remains prevention of heel/foot PUs and plantar flexion contractures.
Evidence-Based Quality Improvement Initiative and Nursing/Physical Therapy Collaboration Results in Decreased Hospital-Acquired Heel Pressure Ulcers
Authors: Frances M. Dyckman MSN, BSN, PHN, APRN-CNS, CWOCN, Christine Love PT, DPT
The prevention of hospital-acquired heel pressure ulcers (HAhPUs) is a major focus of the Triple Aim. The development of HAhPUs is associated with increased patient morbidity and pain, decreased quality of life, extended hospital length of stay, and increased costs. The heel is the second most prevalent anatomic location for pressure-related breakdown.
Public hospitals are faced with patients with complex issues, some of whom are homeless, living in poverty, and/or have high risk factors for HAhPU development. This quality assurance/ performance improvement (QAPI) intervention was implemented to meet the objectives of the Triple Aim, reduce the incidence of HAhPUs, and improve patient outcomes.
Implementation of a Cost-effective Practice for Reducing both Pressure Injury and Healthcare Worker Injury during Patient Repositioning
Author: Deanna Zaganas BSN, RN, WOC
Co-authors: Dana Balassa BSN, RN, CWCN, WOC, Andrea Melendez MSN, RN, CHTP, HTCP, HSMI, RM, and Ray McCoy
Patient care standards for pressure injury (PI) prevention require acute care nurses to reposition patients in bed as often as 6-10 times per shift, a significant source of HCWI risk.
The goal of our project was to:
1) Decrease HCWI during in-bed repositioning, and:
2) Prevent hospital acquired sacral/buttock PI (SBPI)
Pressure Injury (PI) Reduction Initiative in Hemodynamically Unstable Patients
Authors: Roxy Lupien MSN, RN, CNL, CWOCN, CFCN & Rados Stoddard BSN, RN, CWON, CFCN
Performance improvement project initiated for manual turning of hemodynamically unstable patients that were not able to tolerate CLRT at above settings.
WOCNs initiated the patient positioning system (PPS) to aide patients and staff with manual repositioning and ensure a 30 degree turn.
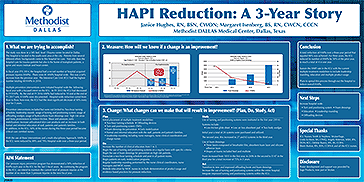
HAPI Reduction: A 3-Year Story
Authors: Janice Hughes RN, BSN, CWON, Margaret Isenberg BS, RN, CWCN, CCCN
The study was done in a 585 bed, level 1Trauma center located in Dallas. Multiple prevention interventions were initiated hospital wide the following fiscal year with a focused intent on the ICU. In FY 2015 the ICU had decreased to 19 HAPIs. By the end of FY 2016 HAPIs had reduced to 10 and at the end of FY 2017 only 4 HAPIs were documented. Hospital-wide reduction varied from floor to floor; how-ever, the ICU had the most significant decrease of 50% every year for 3 years.
With the use of these interventions and a multi-disciplinary Approach, HAPIs in the ICU were reduced by 89% and 79% Hospital wide over a three-year period.
Incontinence Cleansing Protocol Results in 75% Decrease in IAD and 20% Decrease in Facility-Acquired Pressure Ulcers
Author: Rhonda Sullivan PhD, RN, CWON, LNCC
The purpose of this quality improvement initiative was to reduce facility-acquired incontinence-associated dermatitis (IAD) and positively impact facility-acquired pressure ulcers by initiating an evidence-based incontinence care regimen that encompasses a pH–balanced cleanser that moisturizes and protects the skin.
Safe Patient Handling Initiative Results in Reduction in Injuries and Improved Patient Outcomes for Pressure Ulcer Prevention
Author: Heather Way RN, BSN, MSN
A safe patient handling quality improvement (QI) initiative was developed to help ensure appropriate patient repositioning for HAPU prevention, while at the same time preventing caregiver injuries associated with repositioning.
Protecting Skin While Saving Butts, Backs and Bucks
Author: Susie Lee BSN, RN, WCC
Leahi is a 115 bed long-term care facility. In 2015, Leahi had three (3) Patient Handling Injuries (PHIs) at a total cost of $27,003. Total Days Away: 165 (78 restricted)
Objective to introduce an air-assisted repositioning system that would safely assist healthcare workers with less exertion.
Four Years of Heel Pressure Ulcer Prevention
Authors: Debbie Hanna-Bull RN, BScN, MN, Stephen Martin MD FRCS(c), Joan Maclean, OT Reg(Ont)
Heel pressure ulcers (hPUs) are associated with increased morbidity, decreased quality of life, increased costs, and can lead to increased risk for osteomyelitis and other related complications.
This poster represents a sustainable QI intervention, which has led to a 72% reduction in facility-acquired.
Intensive Care Unit Quality Improvement Initiative Decreases Incidence of Hospital-Acquired Pressure Ulcers
Authors: Kelly Chapman MS, RN, CWOCN, Christine Nolan MS, RN, Karen Colegrove MS, RN, CCRN
A quality improvement (QI) initiative was implemented in an intensive care unit (ICU) to prevent HAPUs. This case history describes the methods and results associated with this QI intervention.
Quality Improvement Efforts Result in Pressure Injury Prevention on Adult Critical Care Unit
Authors: Liz Emery RN, MSN, MBA, Lisa Burnett RN, BSN, and Amber Shearn RN, MSN, MBA
The following case history describes a continuous quality improvement (QI) intervention designed to enhance existing HAPI prevention efforts in the critical care unit (CCU).
Ongoing Continuous Quality Improvement Efforts at a Veterans Health Administration Hospital Result in Decreased Incidence of Pressure Injuries
Authors: Imelda S. Hildebrecht MS, APN, NP-C, CWOCN
A quality improvement (QI) initiative was developed at the Federal Health Care Center in North Chicago to adhere to the recommendations of the OIG and prevent the development of PIs in critically ill patients.
28996