Healthcare-acquired infections
Hospitalized patients are at risk for a variety of healthcare-acquired infections. These infections can have an enormous impact on patients and the hospital from a personal and financial perspective. This section provides education and resources to create awareness of various healthcare-acquired infections and the latest evidence-based guidelines and recommended practices for prevention and treatment.
CDC NHSN Keys to success
The National Healthcare Safety Network’s analysis quick reference guide:
- Let’s talk p-value
- And how about that 95% Confidence Interval (CI)?
- Presenting the Standard Infection Ratio (SIR)
CDC Targeted Assessment for Prevention Strategy
TAP Strategy ‘How To’ Guide. This guide will address the following steps of the TAP strategy:
- Running TAP Reports
- Interpreting TAP Reports to Target Specific Units within the Facility
- Communicating TAP Report Data to Engage Facility Leadership and Administrators
- Assessing the Gaps in Infection Prevention
- Implementing Infection Prevention Strategies
NHSN Patient Safety Component Manual
National Healthcare Safety Network Patient Safety Component includes four modules that focus on events associated with medical devices, surgical procedures, antimicrobial agents used during healthcare, and multidrug resistant organisms.
CDC NHSN: A Guide to the SIR
The Standardized Infection Ratio (SIR) is the primary summary measure used by the National Healthcare Safety Network (NHSN) to track healthcare-associated infections (HAIs). As NHSN grows, both in its user-base and surveillance capability, the SIR continues to evolve. Highlighting the SIR and changes resulting from an updated baseline, this document is intended to serve both as guidance for those who are new to this metric as well as a useful reference for more experienced infection prevention professionals.
What the experts say: Hospital tap water & basin water contamination
Research increasing indicates that patient bath basins are a source of bacteria and pose a threat of cross contamination. Bacteria exist in hospital water supplies and hospital staff can transmit bacteria both into and via water. In addition, reusable washcloths can spread harmful bacteria during bathing when bacteria are transferred to the basin and returned to the patient. Patients who have surgical wounds or skin breakdown are prone to acquire HAIs from bath water.
Educational Courses
Strategies to Reduce the Incidence and Complications of Catheter-Associated Urinary Tract Infections
The intended audience for this course is nurses whose practice includes the care of patients with catheters.
Learning objectives
- List three complications associated with indwelling urinary catheters, or IUCs
- Identify sources of urinary catheter contamination
- Describe how the use of bath basins can contribute to catheter contamination
- Identify three practices called for by catheter-associated urinary tract infections, also known as CAUTI, prevention guidelines and lastly,
- List alternatives to IUCs
White papers
Contamination of Hospital Basins
Bacteria is present and proliferating in many areas of the hospital. One area that is particularly problematic is the hospital’s water source. As with any other healthcare-associated infection, occurrence of a hospital-acquired waterborne infection can erode the public’s confidence in healthcare facilities. It is recommended that hospitals implement water-safety programs; the solution to the problem, however, is extensive and not always feasible. There are cost-effective ways to eliminate the exposure of vulnerable patients to the potentially lethal effect of contaminated water. One such method is to replace the use of hospital water in the very fundamental practices of patient hygiene. The elimination of the need to use tap water for performing tasks such as daily bathing and incontinence clean-up can help reduce the exposure to harmful pathogens that may be hiding in the water source, unbeknownst to the staff and patients. This method can also eliminate a common source of bacteria, the bath basin.
Implementation tools
What the experts say: Meatal cleansing for the foley catheterized patient
Standards for proper meatal cleansing are not well-defined, which can lead to process variation. In addition to being inconsistent, traditional incontinence cleanup methods increase the risk of cross contamination from basins – a proven CAUTI risk factor – and waterborne hospital-acquired infections.
What the experts say: Hospital tap water & basin water contamination
Research increasing indicates that patient bath basins are a source of bacteria and pose a threat of cross contamination. Bacteria exist in hospital water supplies and hospital staff can transmit bacteria both into and via water. In addition, reusable washcloths can spread harmful bacteria during bathing when bacteria are transferred to the basin and returned to the patient. Patients who have surgical wounds or skin breakdown are prone to acquire HAIs from bath water.
Posters
Bath Basin Elimination: Removing the bath basin to reduce catheter-associated urinary tract infection in critically ill patients
Authors: Natalia Cineas, DNP, RN, NEA-BC, Rosalyn Beswick, RN, MSN ANP-BC CWOCN, Maria Vezina, EdD, RN, NEA-BC
The purpose of this study was to compare the effectiveness of two methods of patient bathing and incontinence care on overall cost and patient outcomes for catheter-associated urinary tract infections (CAUTI) in critically ill patients.
Patient’s Bath Basin: Friend or Foe
Authors: Noreen Johnson RN, BSN, CIC, Sharon Williamson MT(ASCP)SM, CIC, Barbara Danielson RN, BSN, CIC
A point prevalence study was conducted on 20 bath basins of patients who were bedbound from 2 separate nursing units (Medical/Surgical & ICU). All bath basins were emptied of contents and cultured using a sterile sponge by one nurse. After labeling the sponge, it was mailed to an outside laboratory.
Case studies
CNS impact through innovation and implementation of PrimaFit™ External Urine Management System for Females
Terrie Beeson and Carmen Davis are Clinical Nurse Specialists at University Hospital, a part of Indiana University Health System. In an effort to reduce CAUTI prevalence and harm, Beeson and Davis evaluated strategies designed to help decrease indwelling urinary catheter usage in female patients.
Implementation tools
What the experts say: The impact of Surgical Site Infections (SSI) and hospital-acquired pneumonia (HAP)
Surgical site infections (SSIs) are one of the most common healthcare-acquired infections and one of the most costly. SSIs occur after 2% to 5% of all inpatient surgeries, amounting to 160,000-300,000 SSIs/year. SSIs can also add 7-11 days to a patient’s length of stay and increase costs and mortality risk. This has a dramatic impact on a patient’s quality of life and leads to never events that impact the facility.
Posters
A Novel Immediate Pre-Operative Decolonization Strategy Reduces Surgical Site Infections
Authors: E. Bryce, T. Wong, D. Roscoe, L. Forrester, B. Masri
Bacterial decolonization (DcTx) prior to surgery decreases the risk of surgical site infections (SSIs). Traditional DcTx consist of chlorhexidine (CHG) +/- intranasal mupirocin.
A novel approach using immediate preoperative DcTx with intranasal photodisinfection therapy (PDT) and CHG body wipes was assessed.
Objectives to determine if immediate DcTx using PDT and CHG reduces SSI rates and to determine if immediate DcTx can be integrated into pre-operative work flow.
The Effect of Universal Intranasal Povidone Iodine Antisepsis on Total Joint Replacement Surgical Site Infections
Authors: Lynne Brown RN, BSN, MBA, CIC, Mark Shelly MD, Linda Greene RN, MPS, CIC, Anne Marie Pettis RN, BSN, CIC, Sherry Romig RN
Post-operative infections are infrequent after total joint arthroplasty. When they do occur however, they result in significant morbidity. Colonization with Staphylococcus aureus (SA) increases the risk for surgical site infections (SSI). Previous studies have shown that Mupirocin reduces SA infections in those patients who are colonized. However, mupirocin resistant SA is increasingly being reported. Therefore preoperative intranasal povidone iodine (PI) was implemented in a busy orthopedic service as an alternative to mupirocin to assess the effect on infection rates from all pathogens.
Revisiting Process Improvement for Total Joint Arthroplasty Surgical Site Infections
Authors: Marcia L. Waibel MBA, MT(ASCP), CIC
A Lean Process Improvement Kaizen Event in 2009 for Total Hip Arthroplasty (THA) addressed an increase in total hip surgical site infections. Processes were standardized to best practice, resulting in a sustained reduction in infections.
In early 2010, the processes developed for THA were adopted for Total Knee Arthroplasty (TKA). By the end of 2011, the process was no longer in control, as evidenced by an increase in both THA and TKA infections.
Concurrent efforts were launched to address the issue and restore the low infection rates that resulted from the 2009 process improvement.
Perioperative Antisepsis Protocol Initiative
Authors: Burgandi Thompson LPNII, Nancy Aming RN, BSN, MSHA, BC, Margaret Parr RN, BSN, CIC
Departmental collaboration with Infectious Control found literature review resulting with implementation of evidence based practice.
Interdepartmental perioperative antisepsis protocol development with Infectious Control, PACU Leadership team, and Informatics Systems.
Fully implemented at ORMC by March 2013 for all skin incisional procedures.
Educational Courses
Evidence-Based Practices for Comprehensive Oral Care, Part 1: Anatomy and Physiology
Learning objectives
At the completion of this activity you should be able to:
- List the components of the anatomy and physiology of the oral cavity
- Describe how oral cavity health impacts overall health
- List the structures of the oral cavity and the areas prone for bacterial colonization
Evidence-Based Practices for Comprehensive Oral Care, Part 2: Complications
Learning objectives
At the completion of this activity you should be able to:
- Describe the impact of oral health to a patient’s overall well-being
- List the potential side effects of medication to the oral cavity
- Discuss the role of oral plaque bacteria in the development of health conditions
- Describe the components of a thorough oral cavity assessment
- List common Health conditions that have potential impact to oral health
Evidence-Based Practices for Comprehensive Oral Care, Part 3: Guidelines and Interventions
Learning objectives
At the completion of this activity you should be able to:
- Discuss the impact of hospital-acquired pneumonia and ventilator-associated pneumonia on hospital quality and patient outcomes
- List the evidence-based recommendations for the prevention of hospital-acquired pneumonia
- Describe the nursing interventions geared toward management of oral dysfunction
Implementation tools
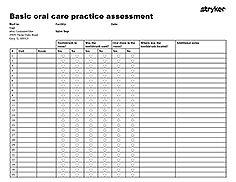
Basic oral care practice assessment
Downloadable resource to review:
- Toothbrush in room?
- Toothbrush used?
- Oral rinse in room?
- Location
What the experts say: Cetylpyridinium Chloride as an oral antiseptic
Leading healthcare institutions and organizations have adopted protocols for oral care as part of their strategies to address hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP). These oral care protocols follow a comprehensive approach aimed at key reservoirs for bacteria on the teeth as well as within the oral cavity and oropharynx.
One common and consistent element of these protocols is the use of an oral antiseptic, such as Cetylpyridinium Chloride (CPC). The following institutions recommend the use of 0.05% CPC as part of a comprehensive oral care protocol to address key risk factors that are known to lead to HAP and VAP.
What the experts say: The impact of Surgical Site Infections (SSI) and hospital-acquired pneumonia (HAP)
Surgical site infections (SSIs) are one of the most common healthcare-acquired infections and one of the most costly. SSIs occur after 2% to 5% of all inpatient surgeries, amounting to 160,000-300,000 SSIs/year. SSIs can also add 7-11 days to a patient’s length of stay and increase costs and mortality risk. This has a dramatic impact on a patient’s quality of life and leads to never events that impact the facility.
What the experts say: The role of 0.12% Chlorhexidine Gluconate Oral Rinse (CHG) in the ventilated patient
Leading healthcare institutions and organizations have adopted protocols for oral care as part of their bundle of strategies used to address hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP). These oral care protocols follow a comprehensive approach aimed at key reservoirs for bacteria on the teeth as well as within the oral cavity and oropharynx. One common and consistent element of these care bundles is the inclusion of 0.12% Chlorhexidine Gluconate (CHG) oral rinse. The following institutions recommend the use of 0.12% CHG as part of a comprehensive oral care protocol to address key risk factors that are known to lead to HAP and VAP.
What the experts say: The role of pneumonia and sepsis
Leading institutions in healthcare recognize sepsis as a significant challenge. Sepsis is a blood stream infection that creates a cascade of bodily responses, which can ultimately result in organ failure and/or death. Sepsis is one of the leading causes of death in the United States, with a 34.7 to 52% mortality rate in hospitals. Sepsis affects more than one million people a year and causes 258,000 deaths annually in the U.S. Furthermore, the treatment of sepsis costs the U.S. healthcare market $24 billion per year, making it the number one hospitalization cost in the country. Individually, sepsis costs an average of $20,000 - $40,000 per hospital stay. While any infection can lead to sepsis, respiratory infections are the most common precipitating condition. Below is a summary of some of the evidence highlighting the relationship between pneumonia and sepsis.
Posters
Non-Ventilator Hospital-Acquired Pneumonia (NV-HAP) in the ICU: Incidence and Prevention
Authors: Barbara Quinn RN, ACNS-BC, Dian Baker RN, PhD, Carol Parise PhD
Currently, there are no requirements to monitor NV-HAP. Limited studies available indicate that NV-HAP is an emerging factor in prolonged hospital stays of 7-9 days, patient mortality of 19.8%, and increased cost of $40,000. New studies by Esperatti (2010) and Davis (2012) indicate that VAP and NV-HAP share similar pathogens and mortality rates, and NV-HAP occurs more frequently than VAP.
Hospital-acquired pneumonia is generally considered a preventable condition, and may be subject to loss of reimbursement in the future.
This was a descriptive, quasi-experimental study using retrospective data to determine the incidence, demographics, and clinical factors of NV-HAP. NV-HAP data were obtained from a large, urban hospital’s electronic integrated medical management system.
Ventilator-Associated Pneumonia Prevention How Oral Care Helps Reduce VAP Rates
Authors: Angi Bollinger, Michele Berry, Christa Brecht, Kristen Conro, Kim Hunt, Susie Kuretski, Barb Patterson
Ventilator-associated pneumonia (VAP) is a nosocomial infection defined as a pneumonia arising more than 48 hours after endotracheal intubation and the initiation of mechanical ventilation.
VAP has an in-hospital mortality rate as high as 50% and increases hospital length of stay by as much 13 days per patient, with an estimated cost of up to $40,000 per case.
After an increase in VAP rates, the ICU Practice Council initiated a new VAP prevention protocol in an effort to achieve best practice.
Clinical Attributes of Non-Ventilator Associated Hospital-Acquired Pneumonia (NV-HAP)
Authors: Barbara Quinn MSN, ACNS-BC, Dian Baker PhD, APRN, Carol Parise PhD
Multiple studies demonstrate the incidence of ventilator associated pneumonia and the effectiveness of a ventilator bundle for prevention. However, there are no requirements to monitor or report NV-HAP.
Limited NV-HAP studies indicate that it is an emerging factor in hospital-acquired infections. NV-HAP may result in increased morbidity and increased costs up to $40,000/ case.
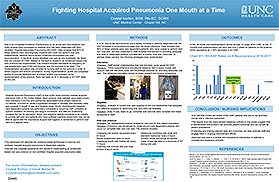
Fighting Hospital Acquired Pneumonia One Mouth at a Time
Author: Crystal Norton BSN, RN-BC, SCRN
Hospital Acquired Pneumonia (HAP) is one of the most common hospital acquired infections (HAI) in the United States. More common than catheter associated urinary tract infections (CAUTIs) and central line associated blood stream infections (CLABSIs), is known to cause a significant increase in mortality and morbidity rates, and increase in length of stay and hospital costs.
Acute, neurologically impaired, care dependent patients are particularly vulnerable to acquiring HAP. Limitation of speech, limitation of chewing and tongue movement, and difficulty swallowing increase the risk for aspiration. Motor and cognitive deficits contribute to an inability to provide self-care and patients who have suffered cognitive impairment may not be able to appreciate the importance of good oral hygiene or remember to perform oral care on a regular basis.
Implementation tools
What the experts say: Incontinence care and pressure injury prevention
Incontinence-Associated Dermatitis (IAD) is defined as “an inflammation of the skin that occurs when urine or stool comes into contact with perineal or perigenital skin.” IAD is also a major risk factor for pressure ulcers.
Posters
Barrier Cream Cloth Efficacy and Prevention of Transepidermal Water Loss-An Important Consideration in Product Selection
Author: Dennis P. West PhD, FCCP, CIP
In establishing evidence for skin barrier efficacy afforded by products that utilize disposable wipes for leave-on application, Transepidermal Water Loss (TEWL) is a well-accepted method for assessing skin barrier efficacy.
With product effectiveness as a critical component to clinical decision-making, the aim of this study is to examine the differences in ability to prevent TEWL by four currently-marketed barrier wipes that vary in dimethicone concentration (0% to 3.6%) and that utilize leave-on application.
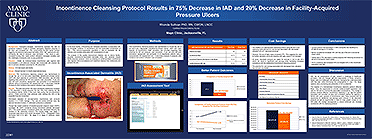
Incontinence Cleansing Protocol Results in 75% Decrease in IAD and 20% Decrease in Facility-Acquired Pressure Ulcers
Author: Rhonda Sullivan PhD, RN, CWON, LNCC
The purpose of this quality improvement initiative was to reduce facility-acquired incontinence-associated dermatitis (IAD) and positively impact facility-acquired pressure ulcers by initiating an evidence-based incontinence care regimen that encompasses a pH–balanced cleanser that moisturizes and protects the skin.
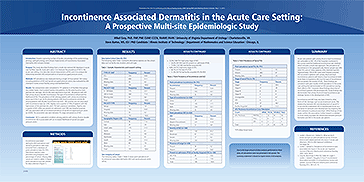
Incontinence Associated Dermatitis in the Acute Care Setting: A Prospective Multi-site Epidemiologic Study
Authors: Mikel Gray PhD, FNP, PNP, CUNP, CCCN, FAANP, FAAN and Steve Bartos MS, ED
Despite a growing number of studies, knowledge of the epidemiology, etiology, pathophysiology, and clinical characteristics of Incontinence Associated Dermatitis (IAD) remains limited.
This study describes findings from a multi-site national IAD database in acute care facilities. Specific study aims were: 1) to measure the prevalence of IAD in the acute care setting, 2) to describe clinical characteristics of IAD, and 3) to analyze the relationship between IAD and prevalence of sacral/coccygeal pressure ulcers.
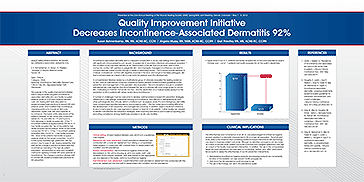
Quality Improvement Initiative Decreases Incontinence-Associated Dermatitis 92%
Authors: Susan Bohnenkamp RN, MS, ACNS-BC, CCM, Angela Muzzy RN, MSN, ACNS-BC, CCRN, Gail Priestley RN, MS, ACNS-BC, CCRN
The purpose of this quality improvement initiative was to reduce facility-acquired incontinence associated dermatitis (IAD) and facility-acquired pressure ulcers on a 20-bed medical intensive care unit. Nursing staff were educated on evidence-based best practices to prevent IAD and pressure ulcers, and modified their incontinence cleansing protocol to include an all-in-one, disposable, barrier cloth with each episode of incontinence.
First Steps in Cultivating Incontinence-Associated Dermatitis Prevention Practices in One Local Health District
Authors: Michelle Barakat-Johnson RN, MN PhD Candidate, Michelle Lai MRes PhD Candidate, Timothy Wand RN NP MN(Hons) PhD Associate Professor, Kathryn White RN, MN PhD Professor
A cross-sectional study across 12 wards in four hospitals to examine the prevalence of incontinence and IAD, as well as to determine evidence-into-practice gaps.
Evidence-based initiatives led to a significant reduction in IAD (p = .015), and improvement to the nature of incontinence nursing practices (p < .001). Healthcare strategies, guided by an implementation science framework, enhanced the effectiveness of translating evidence-into-practice and positively assist clinicians to promote optimal patient care.
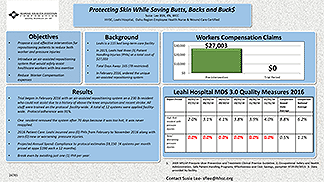
Protecting Skin While Saving Butts, Backs and Bucks
Author: Susie Lee BSN, RN, WCC
Leahi is a 115 bed long-term care facility. In 2015, Leahi had three (3) Patient Handling Injuries (PHIs) at a total cost of $27,003. Total Days Away: 165 (78 restricted)
Objective to introduce an air-assisted repositioning system that would safely assist healthcare workers with less exertion.
28996