Strategies to prevent Catheter-Associated Urinary Tract Infections (CAUTIs)
22-Aug-2024

4-minute read
Society for Healthcare Epidemiology (SHEA) 2022 update: a collaborative effort that integrates best practice into the safe delivery of patient care
Laurie Mai, MSHQS, BSN, RN
Insights from the latest Compendium
The Compendium, sponsored by the Society for Healthcare Epidemiology of America (SHEA), offers updated guidance for hospitals to help reduce the risk of catheter-associated urinary tract infections (CAUTIs). This Compendium is the first update since 2014 and features insights from over 100 global specialists. Key contributors include SHEA, the Infectious Diseases Society of America, the Association for Professionals in Infection Control, The Joint Commission, and the American Hospital Association.
Multidisciplinary strengths and best practices
A notable feature of this Compendium is its multidisciplinary approach, making it invaluable for providers, nurses, medical students, and residents. By reviewing and applying these updated recommendations, healthcare professionals can help ensure that best practices guide patient care.
The preventable burden of CAUTIs
The Compendium clearly outlines the associated risks of CAUTIs. Alarmingly, about 50% of urinary catheters in hospitalized patients may not be needed.1 Once a catheter is placed, CAUTIs become a common complication, with roughly 40% directly linked to their presence.1 The daily risk of bacteriuria ranges from 3% to 7%, making the duration of catheterization the most significant risk factor.1 Therefore, deciding when to use an indwelling urinary catheter and removing it promptly when no longer necessary is crucial.
The vital role of nurses in CAUTI prevention
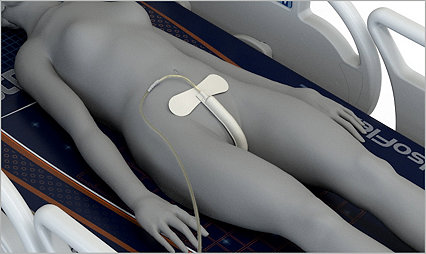
Nurses play a critical role in preventing CAUTIs, being the primary professionals responsible for inserting, maintaining, and removing urinary catheters. The Compendium's "Essential Practices" section advises the healthcare team, including nurses, to conduct daily assessments of all patients with a urinary catheter. This assessment considers alternatives to indwelling catheters, such as straight catheters, non-catheter incontinence management supplies, and external urinary devices for both men and women.
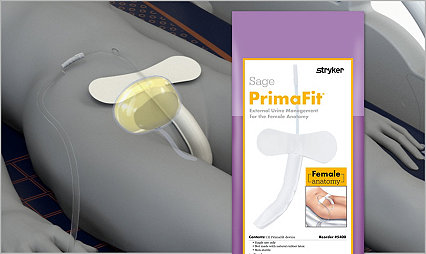
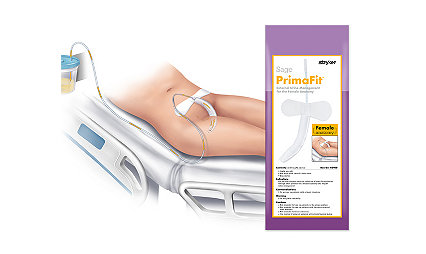
Successful reduction of CAUTIs with external urinary devices
The Compendium references several studies showing success in reducing CAUTIs through external urinary devices (EUDs). Researchers emphasize that robust education is crucial for this success. After evaluating the selected EUDs, a plan can be developed to introduce the product on nursing units. Collaboration with nurse educators, wound care nurses, infection preventionists, and product representatives ensures professional nurses and technicians receive individual instruction on using and maintaining EUDs. Nurse EUD "champions" are highly recommended to provide ongoing support and education.
Evidence-based recommendations and antimicrobial stewardship
Recommendations in the Compendium are classified based on evidence quality (low, moderate, or high) and include several points specific to infection prevention. A new topic since the 2014 update is antimicrobial stewardship, addressing the high rate of unnecessary urine cultures in hospitals. The Compendium offers strategies to reduce these unnecessary tests, including establishing criteria for ordering urine cultures.
Practices to avoid and unresolved issues
The Compendium also highlights approaches that should not be used in acute care hospitals, such as routine use of antimicrobial or antiseptic-impregnated catheters and routine screening for asymptomatic bacteriuria. Unresolved issues include the choice between antiseptic solution and sterile saline for cleaning before catheter insertion and the routine replacement of catheters in place for more than 30 days.
Visual tools for reducing CAUTIs and urethral injury
A helpful visual included in the Compendium precisely addresses ways to reduce CAUTIs and prevent traumatic injury to the urethra.

Patel PK, Advani SD, Kofman AD, et al.,(2023) Strategies to prevent catheter-associated urinary tract infections in acute-care hospitals: 2022 Update, Infection control and hospital epidemiology, 44(8), 1209–31.
Collective goal: zero harm
CAUTIs remain a significant healthcare concern, and hospitals are challenged to focus on eliminating them. With zero harm to patients as our collective goal, we must work together to implement these updated strategies to keep patients free from hospital-acquired CAUTIs.
Learn more about our external urinary management systems
At Stryker, we’re dedicated to improving patient safety and quality of care. To learn more about our external urinary management products, click here.
Related news
Reduce the risk of catheter-associated urinary tract infection (CAUTI) in hospitals
Catheter-associated urinary tract infections (CAUTIs) are among the most common types of healthcare-associated infections, and reducing them is beneficial to hospitals, caregivers and patients.
Learn moreNYC Medical Center Implementation of External Female Catheter avoids $16M in costs over 2 years
In 2018, the implementation of the external female urine management device was introduced as a standard of nursing care as an alternative to an indwelling urinary catheter. Data captured in 2019 and 2020 showed utilization of the external female device to be 36% and 46%, respectively.
Learn moreThe Sage PrimaFit External Urine Management for the Female Anatomy helped decrease CAUTI rates 72%
Learn moreSage PrimaFit External Urine Management System for the Female Anatomy helped reduce CAUTI rate 63%
Catheter-related infections decreased from before the introduction to EUDFA and after. This is not a cause-and-effect relationship, but the trend is promising.
Learn moreReference:
1. Patel PK, Advani SD, Kofman AD, et al.,(2023) Strategies to prevent catheter-associated urinary tract infections in acute-care hospitals: 2022 Update, Infection control and hospital epidemiology, 44(8), 1209–31.
Laurie Mai, MSHQS, BSN, RN is a paid consultant of Stryker. The data included in this presentation was collected by the author of this presentation. The opinions expressed are those of Laurie Mai, MSHQS, BSN, RN and are not necessarily those of Stryker. Individual results may vary.
SAGE-UM-COMM-1201102_REV-0_en_us