Recent study shows sepsis occurred in 20% of NV-HAP patients
30-Mar-2023
American Journal of Infection Control publishes retrospective cohort analysis of VHA data
Non-ventilator hospital acquired pneumonia (NV-HAP) has been widely underappreciated as a hospital-acquired infection and there is a paucity of studies to evaluate its impact on patient outcomes. Using data from the large, comprehensive Veterans Health Administration (VHA) Central Data Warehouse, Carey et al. evaluated the association between NV-HAP and patient outcomes in U.S. Veterans admitted to 133 acute care VHA hospitals. They conducted a retrospective cohort analysis of 1,397,799 acute care admissions which met inclusion criteria for the period between October 2015 and December 2020. The purpose of this study was to identify the difference in 30-day and 1-year associated mortality, length of stay, 12-month costs and inpatient sepsis between patients who developed NV-HAP and those who did not. A secondary purpose was to estimate the probability of developing NV-HAP based on patient demographics, comorbidities, recent medication exposure and diagnoses determined to be present on admission.
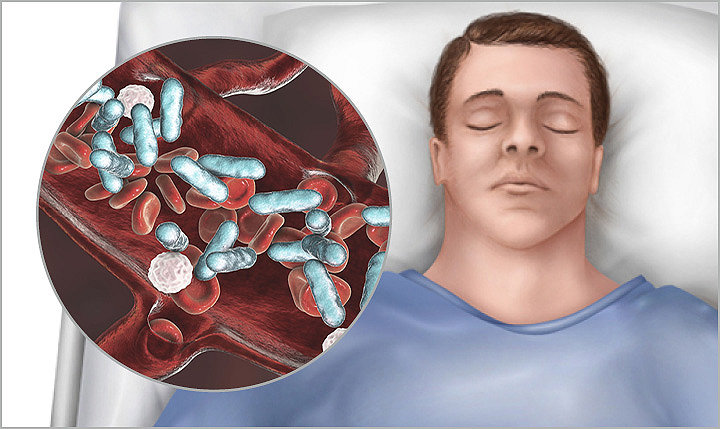
The results demonstrated that of the 1,397,799 admissions evaluated, 8,891 developed NV-HAP (0.6% of admissions) while 1,388,908 (99.4%) did not. A total of 6,792,098 at risk hospitalized days were analyzed and the overall rate of NV-HAP was 0.5 cases per 1,000 hospitalized days. The mean length of stay for NV-HAP was 26.3 days (6.72 non-NV-HAP); 30 day mortality was 18.4% (4.5% non-NV-HAP); and 1-year mortality was 47.8% (21.4% non-NV-HAP). Inpatient sepsis occurred in approximately 20% of NV-HAP admissions (0.7% non-NV-HAP). Total median 12-month medical costs were $138,136 for NV-HAP ($64,357 non-NV-HAP). The secondary purpose was to estimate the probability of developing NV-HAP on admission. Using multiple modeling techniques, variables available on admission were insufficient to adequately identify high and low risk patient groups.
This retrospective cohort study both confirms previous data on NV-HAP outcomes and expands the information on outcomes using relatively current data as compared to previous studies. The burden of NV-HAP is costly both in patient outcomes (mortality, sepsis, length of stay) and economically (direct medical costs). A key take-away is the relationship between the occurrence of NV-HAP and the subsequent development of sepsis. Prior studies have associated NV-HAP and sepsis but have not been able to specifically identify what proportion of all inpatient sepsis was preceded by NV-HAP. Continued research is needed to further our knowledge of patient outcomes, identify successful interventions to prevent this deadly hospital-acquired infection and identify specific patients at risk.
The study by Carey et al. is a major contribution to the literature. Strengths include the use of large, comprehensive database, well-documented methodology and strong analytics. Only a small portion of the results were shared here. The study is data-rich, and one must read the study to truly appreciate all the results. A potential limitation is the use of the VHA population for this study which may limit external reliability (generalizability). However, the impact on external reliability is minimal as gender and race were not strongly associated with NV-HAP risk.
Full article: https://doi.org/10.1016/j.ajic.2022.02.023
Learn more about our oral hygiene products.
Reference: 1. Carey, E., Chen, H. P., Baker, D., Blankenhorn, R., Vega, R. J., Ho, M., Munro, S. The association between non-ventilator associated hospital acquired pneumonia and patient outcomes among U.S. Veterans. American Journal of Infection Control, 2022; 50(12), 1339-1345.
SAGE-OC-COMM-578944_REV-0_en_us
