Information for healthcare professionals
Studies have shown that orthopaedic surgery is a mentally and physically demanding surgical specialty.1
50%
of surgeons experience burnout.2
77%
of surgeons experience back pain.3
74%
of surgeons experience neck pain.3
86%
of surgeons reported at least one MSK condition since training linked to practicing orthopaedics.4
Reimagining the Direct Anterior approach
You can now approach Direct Anterior with less stress and less sweat.
Mako Total Hip and Direct Anterior Reconstructive Technology (DART™) can help you on your journey to reduce, if not eliminate, fluoroscopy.
Less Stress
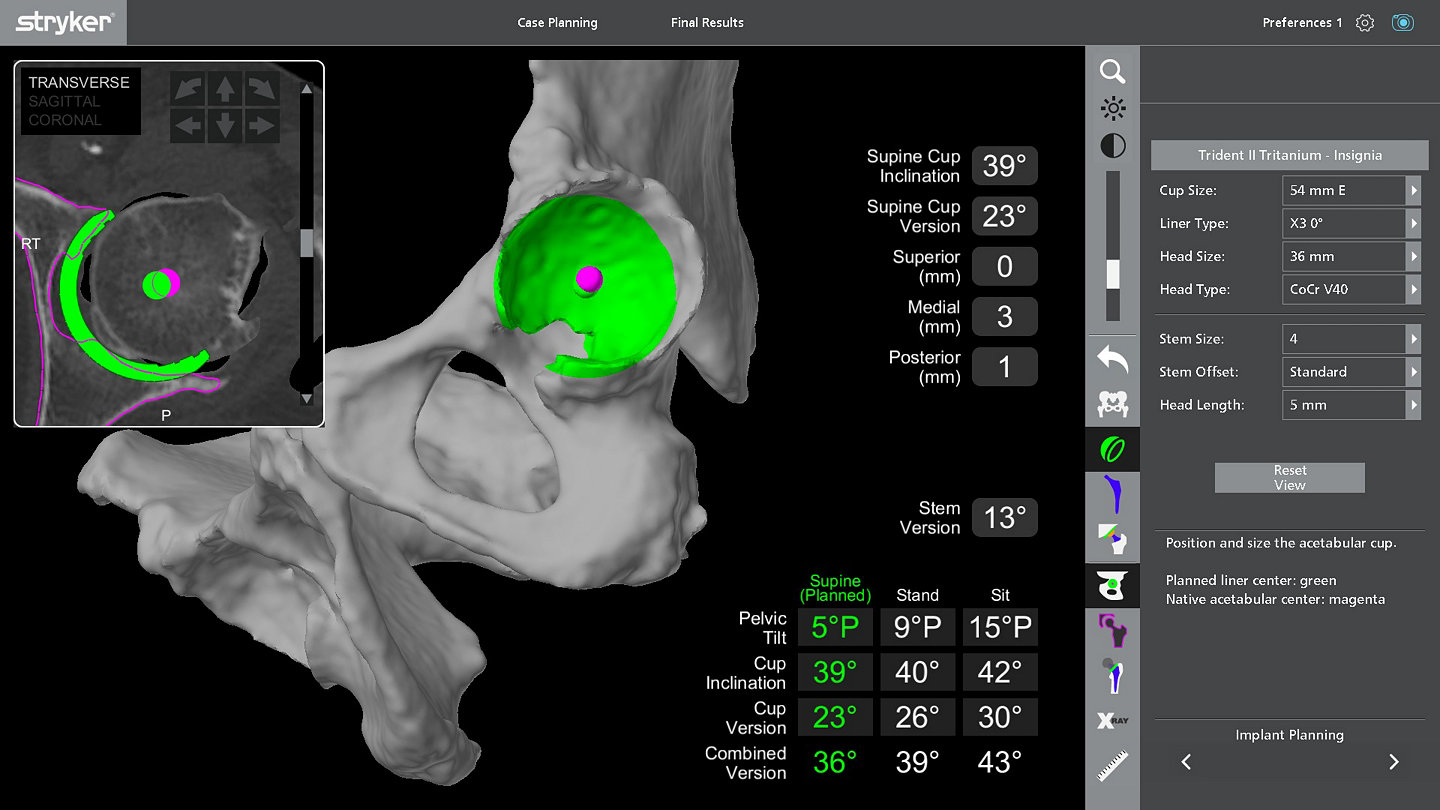
With 3D CT-based planning and AccuStopTM haptic technology, Mako Total Hip and DART help deliver a predictable surgical experience,5-7 providing confidence and reducing stress.8
Less Sweat
Reduce, if not eliminate, your use of fluoro and help drive efficiencies in your workflow so that you can sweat less.8-10

Why join the journey to fluoro free?
Potential concerns associated with fluoroscopy
With the use of fluoroscopy in direct anterior procedures, it’s important to be aware of the potential risks' fluoroscopy may pose for surgeons and OR staff.11
Click below to explore the common concerns:
Join the journey to fluoro free
With Mako Total Hip and DART
Click to explore more
Ready to get started on your journey to fluoro free?
Reduce if not eliminate fluoro
Reduction of fluoro seen in the Direct Anterior workflow
When it comes to the direct anterior approach, where the field of view may be obscured and the use of fluoroscopy may be misleading, knowing more about a patient’s unique anatomy, having guidance while preparing the acetabulum and having a wide range of DA options can make a difference. 22,23
Click below to see how to reduce if not eliminate fluoro in your DA workflow with Mako Total Hip features.
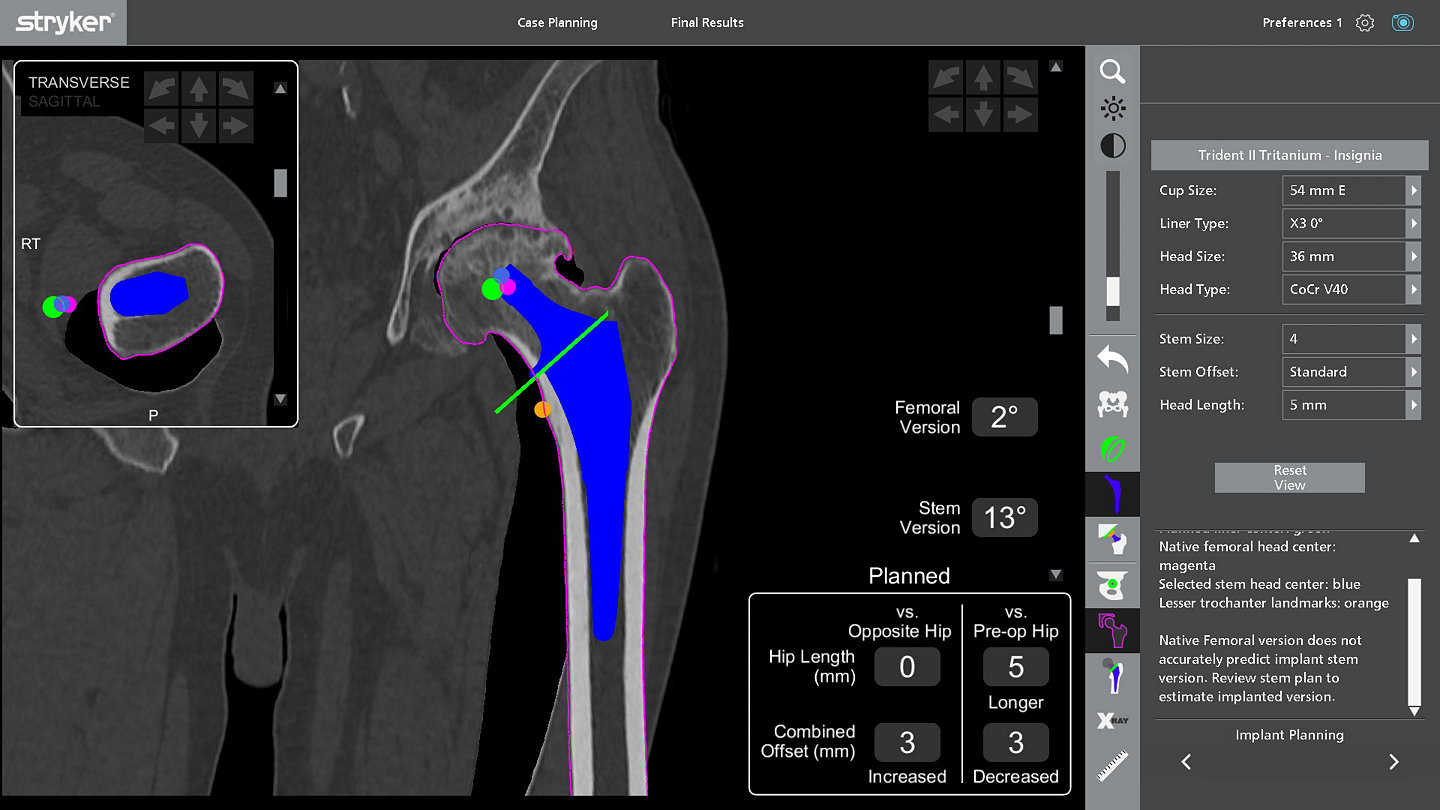
The digital ruler feature allows surgeons to plan their neck cut and measure intraoperatively, to have a more reproducible neck cut and stem placement. 9
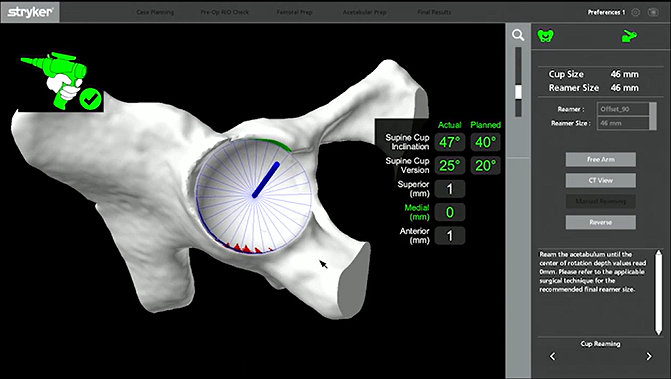
Guided reaming allows surgeons to single stage ream while accurately restoring the center of rotation and achieving accurate bone preparation to plan with Direct Anterior. 5
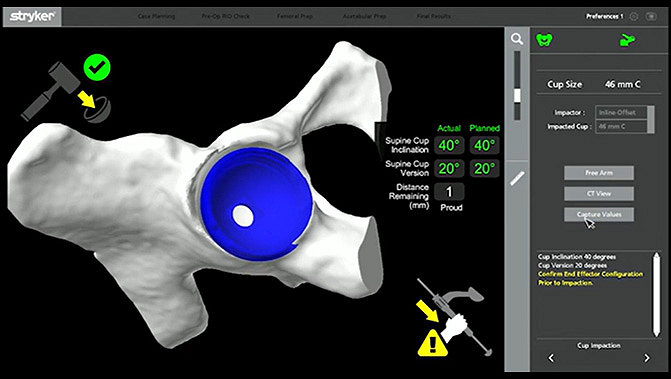
Guided cup placement allows surgeons to implant the cup at the desired inclination and version with Direct Anterior. 5,27
Ability to size stem with in ±1 size due to CT based planning and digital ruler. 28
Intraoperative feedback on hip length and offset can lead to less trialing and has been shown to restore hip length and offset. 29
"Utilizing Mako Total Hip and Stryker’s DART portfolio has allowed me to perform my total hip replacements more accurately to my plan without the need for intraoperative fluoroscopy. This has led to less stress on my body and has allowed me to be more efficient with my direct anterior hips due to not having to rely on intraoperative fluoroscopy."5,8,9,10
- Dr. Charles Claps, D.O.
Dr. Claps is a paid-consultant of Stryker Orthopaedics. The opinions expressed by Dr. Claps are those of Dr. Claps and not necessarily those of Stryker. Individual experiences may vary.
Contact the team
To learn more about joining the journey to fluoro free, contact the team below.
References
- Cohen-Rsenblum AR, Varady NH, Lonovicz O, Chen AF. Repetitive musculoskeletal injuries: a survey of female adult reconstruction surgeons. JoA37 (2022) 1474-1477.
- Daniels AH, DePasse JM, Kamal RN. Orthopaedic Surgeon Burnout: Diagnosis, Treatment, and Prevention. J Am Acad Orthop Surg. 2016;24(4):213- 219. doi:10.5435/JAAOS-D-15-00148
- Lucasti C, Maraschiello M, Slowinski J, Kowalski J. Prevalence of Back and Neck Pain in Orthopaedic Surgeons in Western New York. J Am Acad Orthop Surg Glob Res Rev. 2022 Jan 6;6(1):e21.00252. doi: 10.5435/JAAOSGlobal-D-21-00252. PMID: 34989709; PMCID: PMC8740880.
- Swank KR, Furness JE, Baker E, Gehrke CK, Rohde R. A Survey of Musculoskeletal Disorders in the Orthopaedic Surgeon: Identifying Injuries, Exacerbating Workplace Factors, and Treatment Patterns in the Orthopaedic Community. J Am Acad Orthop Surg Glob Res Rev. 2022 May 1;6(5):e20.00244. doi: 10.5435/JAAOSGlobal-D-20-00244. PMID: 35608969; PMCID: PMC9132526.
- Foissey C, Batailler C, Coulomb R, et al. Image-based robotic-assisted total hip arthroplasty through direct anterior approach allows a better orientation of the acetabular cup and a better restitution of the centre of rotation than a conventional procedure. Int Orthop. 2023;47(3):691-699. doi:10.1007/s00264-022-05624-6
- Hampp EL, Caba M, Scholl L, Faizan A, Frye BM, Nessler JP, Sequeira SB, Mont MA. Can Robotic-Arm Assistance Decrease Iatrogenic Soft-Tissue Damage During Direct Anterior Total Hip Arthroplasty? Surg Technol Int. 2024 Mar 1;44:sti44/1761. Epub ahead of print. PMID: 38442246.
- Di Gangi C, Prinos A, Buehring W, Meere P, Meftah M, Hepinstall MS. Fewer Dislocations after Total Hip Arthroplasty with Robotic Assistance or Fluoroscopic Guidance.J Arthroplasty. Published online July 11, 2024. doi:10.1016/j.arth.2024.07.002
- Caba M, Gains C, Nessler J, Frye B, Scholl L, Sequeira SB, Mont M, Physical and Mental Demand During Direct Anterior Total Hip Arthroplasty: Comparison of Robotic-Assisted and Conventional Techniques. Journal of Orthopaedics. 2024: https://doi.org/10.1016/j.jor.2024.07.001.
- Nessler J, Stephanie C, Barga K, Coppolecchia A. Robotic-Arm Assisted Total Hip Arthroplasty: Worklow Optimization and Operative Times. Surg Technol Int. 2023 Nov 30;43:sti43/1708. doi: 10.52198/23.STI.43.OS1708. Epub ahead of print. PMID:38038176
- Caba M, O’Neill C, Nessler J, Frye B, Scholl L, Sequeira SB, Mont MA, Robotic Assistance is Associated with Improved Surgical Eficiency During Direct Anterior Total Hip Arthroplasty, Journal of Orthopaedics, https://doi.org/10.1016/j.jor.2024.06.027
- Daryoush JR, Lancaster AJ, Frandsen JJ, Gililland JM. Occupational Hazards to the Joint Replacement Surgeon: Radiation Exposure. J Arthroplasty. 2022 Aug;37(8):1464-1469. doi: 10.1016/j.arth.2022.02.095. Epub 2022 Mar 2. PMID: 35247485
- McArthur BA, Schueler BA, Howe BM, Trousdale RT, Taunton MJ. Radiation Exposure during Fluoroscopic Guided Direct Anterior Approach for Total Hip Arthroplasty. J Arthroplasty. 2015 Sep;30(9):1565-8. doi: 10.1016/j.arth.2015.03.029. Epub 2015 Mar 31. PMID: 25873283.
- Jinnai Y, Baba T, Zhuang X, Tanabe H, Banno S, Watari T, Homma Y, Kaneko K. Does a luoro-assisted direct anterior approach for total hip arthroplasty pose an excessive risk of radiation exposure to the surgeon? SICOT J. 2020;6:6. doi: 10.1051/sicotj/2020004. Epub 2020 Feb 18. PMID: 32068533; PMCID: PMC7027395.
- Daryoush JR, Lancaster AJ, Frandsen JJ, Gililland JM. Occupational Hazards to the Joint Replacement Surgeon: Radiation Exposure. J Arthroplasty. 2022 Aug;37(8):1464-1469. doi: 10.1016/j.arth.2022.02.095. Epub 2022 Mar 2. PMID: 35247485
- Valone LC, Chambers M, Lattanza L, James MA. Breast Radiation Exposure in Female Orthopaedic Surgeons. J Bone Joint Surg Am. 2016 Nov 2;98(21):1808-1813. doi: 10.2106/JBJS.15.01167. PMID: 27807113.
- Chou LB, Johnson B, Shapiro LM, Pun S, Cannada LK, Chen AF, Valone LC, Van Nortwick SS, Ladd AL, Finlay AK. Increased Prevalence of Breast and All-cause Cancer in Female Orthopaedic Surgeons. J Am Acad Orthop Surg Glob Res Rev. 2022 May 1;6(5):e22.00031. doi: 10.5435/JAAOSGlobal-D-22-00031. PMID: 35587823; PMCID: PMC9126513.
- Wan RC, Chau WW, Tso CY, et al. Occupational hazard of luoroscopy: An invisible threat to orthopaedic surgeons. Journal of Orthopaedics, Trauma and Rehabilitation. 2021;28. doi:10.1177/22104917211035547
- Joshua R. Daryoush, Alex J. Lancaster, Jeffrey J. Frandsen, Jeremy M. Gililland,Occupational Hazards to the Joint Replacement Surgeon: Radiation Exposure, The Journal of Arthroplasty,Volume 37, Issue 8,2022
- Kellens PJ, De Hauwere A, Gossye T, Peire S, Tournicourt I, Strubbe L, De Pooter J, Bacher K. Integrity of personal radiation protective equipment (PRPE): a 4-year longitudinal follow-up study. Insights Imaging. 2022 Dec 6;13(1):183. doi: 10.1186/s13244-022-01323-3. PMID: 36471171; PMCID: PMC9723036.
- Andrew S, Abdelmonem MR, Kohli S, Dabke H. Evaluation of Back Pain and Lead Apron Use Among Staff at a District General Hospital. Cureus. 2021;13(10):e18859. Published 2021 Oct 18. doi:10.7759/cureus.18859
- Gilat R, Mitchnik I, Beit Ner E, Shohat N, Tamir E, Weil YA, Lazarovitch T, Agar G. Bacterial contamination of protective lead garments in an operating room setting. J Infect Prev. 2020 Nov;21(6):234-240. doi: 10.1177/1757177420947466. Epub 2020 Aug 29. PMID: 33408761; PMCID: PMC7745586.
- Brush PL, Santana A, Toci GR, et al. Surgeon Estimations of Acetabular Cup Orientation Using Intraoperative Fluoroscopic Imagining Are Unreliable. Arthroplasty Today. 2023;20:101109. Published 2023 Mar 7. doi:10.1016/j.artd.2023.101109
- James, C. R., Peterson, B. E., Crim, J. R., Cook, J. L. & Crist, B. D. The Use of Fluoroscopy During Direct Anterior Hip Arthroplasty: Powerful or Misleading? J. Arthroplasty. 33, 1775–1779 (2018).
- Thorne TJ, Wright AR, Opanova MI, Mitsumori LM, Lawton DR, Unebasami EM, Nakasone CK. Impact of intraoperative luoroscopic beam positioning relative to the hip and pelvis on perceived acetabular component position. J Orthop. 2022 Nov 24;35:115-119. doi: 10.1016/j.jor.2022.11.014. PMID: 36467427; PMCID: PMC9712816.
- Delagrammaticas, D. E. et al. Intraoperative evaluation of acetabular cup position during anterior approach total hip arthroplasty: are we accurately interpreting? HIP Int. 30, 40–47 (2018).
- Thorne, T. J. et al. Impact of intraoperative luoroscopic beam positioning relative to the hip and pelvis on perceived acetabular component position. J. Orthop. 35, 115–119 (2023).
- Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329-336. doi:10.1007/s11999-013-3253-7
- Rainey JP, Gililland JM, Marchand K, Taylor K, Mont MA, Marchand RC. Evaluation of an Initial Robotic-Assisted Direct Anterior Approach Cohort Receiving a New Short Metaphyseal Filling Collared Femoral Implant. Surg Technol Int. 2024 Apr 4;44:sti44/1759. doi: 10.52198/24.STI.44.OS1759. Epub ahead of print. PMID: 38573818.
- Jerabek SA, Carroll K, Maratt JD, Mayman DJ, Padgett DE. Accuracy of cup positioning, COR restoration and achieving desired hip length and offset following robotic THA. Presented at: Computer Assisted Orthopaedic Surgery (CAOS) 14th Annual Meeting; June 18-21, 2014; Milan, Italy.
JR-GSNPS-SYK-1421151