08-Apr-2024
Benefits of early mobility in the ICU

5-minute read
Early mobility can help in enhancing patient outcomes in the ICU yet is the top missed area of care by nurses.2
Hospitalized patients who spend an extended period in bed can suffer a variety of unintended consequences, including loss of muscle strength at a rate of 20 percent per week of immobility. This immobility can cause degradation of respiratory, cardiovascular, musculoskeletal and gastrointestinal functioning.3 Research indicates that early mobilization in the ICU can help lessen the duration of mechanical ventilation, decrease the risk of ventilator-associated pneumonia, and improve overall patient survival rates.4 By advocating for physical activity, early mobility aids in preventing muscle wasting and maintaining joint range of motion while boosting cardiovascular function.
83%
of a patient’s stay in the hospital is spent lying in bed.1
Physiological impacts of early mobilization in the ICU
Early mobilization in the ICU brings several physiological benefits that contribute to the overall well-being of patients including improvements in respiratory function, cardiovascular health and musculoskeletal strength and function.
Immobility and prolonged bed rest can lead to decreased lung capacity and increased risk of respiratory complications. By encouraging patients to engage in early mobilization activities, such as sitting on the edge of the bed or performing simple exercises, the lungs are actively engaged, promoting better airway clearance and preventing atelectasis.5
Prolonged bed rest can also cause muscle atrophy, weakness and joint stiffness.6 By incorporating early mobilization exercises, patients can regain muscle strength, prevent contractures and maintain joint flexibility – helping to prevent intensive care unit acquired weakness (ICUAW).7
Challenges to implementing early mobility in the ICU
Implementing early mobility in the ICU can be challenging for healthcare professionals due to various barriers. These barriers can hinder the promotion of early mobilization, which is crucial for patients' recovery and overall well-being.
One of the main challenges faced by healthcare professionals is the fear of causing harm or injury to critically ill patients. ICU patients are often fragile and require careful monitoring, making it difficult to initiate early mobility interventions. Additionally, healthcare professionals may be apprehensive about potential additional complications that could arise during mobilization.
Another barrier is the lack of awareness and education among healthcare professionals regarding the benefits of early mobility. Limited knowledge about the positive impact of early mobilization on patient outcomes can hinder its implementation in the ICU setting. It is important for healthcare professionals to be educated about the advantages and evidence supporting early mobility.
To overcome these barriers and facilitate early mobilization, healthcare professionals can employ various strategies. One strategy is to establish clear protocols and guidelines for early mobility in the ICU. These protocols can provide a framework for healthcare professionals to follow, ensuring safe and effective mobilization practices.8
Interdisciplinary collaboration is also crucial in overcoming barriers to implementing early mobility. By working together, healthcare professionals from different disciplines can share their expertise and knowledge, leading to a comprehensive approach to patient care. This collaboration can help address concerns, share best practices and help ensure that early mobility is implemented consistently and effectively.
Prescribing and intervening in early mobilization
Prescribing early mobilization in the ICU involves considering various factors to ensure safe and effective interventions. By tailoring interventions to individual patient populations, healthcare professionals can maximize the benefits of early mobility. Factors influencing the prescription of early mobilization include the patient's overall condition, severity of illness and stability.8 It is crucial to assess the patient's cardiovascular and respiratory systems, as well as their neurological and musculoskeletal functions. This assessment helps determine the level of mobility that can be safely prescribed. Safe and effective interventions for early mobility in the ICU encompass a range of activities. These may include passive range of motion exercises, bed exercises, sitting at the edge of the bed and standing with assistance. Gradually progressing to walking and ambulation, with the support of healthcare professionals, can further enhance the benefits of early mobilization.
Evidence and research supporting early mobility in the ICU
Early mobility in the ICU has garnered significant attention in recent years due to its numerous benefits for patients. Several studies have provided evidence to support the benefits of early mobility in improving patient outcomes and reducing complications.4, 7-9 Furthermore, early mobility has been shown to improve muscle strength and function in ICU patients. A study found that early mobilization led to increased muscle strength and improved functional outcomes among ICU patients, allowing them to regain independence and reduce the risk of long-term disability.9 Based on the accumulating evidence, current guidelines and recommendations emphasize the importance of early mobility in the ICU. The Society of Critical Care Medicine (SCCM) recommends implementing early mobility protocols in the ICU to minimize the negative effects of immobility including delirium.10
Executing early mobility programs in the ICU
Implementing early mobility programs in the ICU can bring numerous benefits for both patients and healthcare professionals. By incorporating specific steps, training and monitoring, hospitals can ensure the successful execution of these initiatives.
The first step in developing an early mobility program is to create a multidisciplinary team consisting of doctors, nurses, physical therapists and other healthcare professionals.8 This team will collaborate to develop protocols and guidelines for early mobility, taking into consideration the unique needs and limitations of ICU patients.
Training and education for healthcare professionals are crucial to the success of early mobility programs. It is essential that the team members are knowledgeable about the benefits of early mobility, the appropriate techniques and equipment to use, and the potential risks and precautions.
Monitoring and evaluating the impact of early mobility initiatives is vital to ensure continuous improvement. By collecting data on patient outcomes, such as reduced length of stay, decreased complications, and improved functional outcomes, hospitals can assess the effectiveness of their early mobility programs.
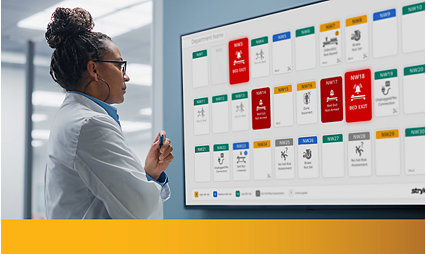
Partners in prevention
Stryker’s innovative solutions help drive improved patient and caregiver outcomes across the continuum of care by helping to address preventable hospital-acquired conditions and enhancing operational workflow. Specifically, our ProCuity ZMX hospital bed system was designed to help enhance safety and care in the ICU while delivering an advanced experience for care teams.
Please reach out to connect with an expert in your area.
Related products
ProCuity ZMX
Designed to enhance safety and outcomes in the ICU while delivering a better experience for nurses and medical teams, with a focus on helping to reduce pressure injuries and supporting early mobility.
Learn moreProCuity LEX / ZX
Designed to enhance safety and outcomes in MedSurg while delivering a better experience for care teams, with a focus on supporting fall prevention protocols.
Learn moreConnected solutions
With simplified workflows and improved communication—hospitals can create richer, more human connections between care teams, patients and their loved ones for safer medical care and improved clinical outcomes.
Learn more1. Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults.J Am Geriatr Soc. 2009;57(9):1660-1665
2. Kalisch, B.J., Tschannen, D., Lee, K.H., “Missed Nursing Care and Patient Falls,” Journal of Nursing Care Quality, Vol. 27 (Jan-Mar 2012)
3. Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 13 Mobility. Available from: https://www.ncbi.nlm.nih.gov/books/NBK591828/
4. Zang K, Chen B, Wang M, Chen D, Hui L, Guo S, Ji T, Shang F. The effect of early mobilization in critically ill patients: A meta-analysis. Nurs Crit Care. 2020 Nov;25(6):360-367. doi: 10.1111/nicc.12455. Epub 2019 Jun 20. PMID: 31219229.
5. Jang, M. H., Shin, M. J., & Shin, Y. B. (2019). Pulmonary and Physical Rehabilitation in Critically Ill Patients. Acute and critical care, 34(1), 1–13. https://doi.org/10.4266/acc.2019.00444
6. Parry, S. M., & Puthucheary, Z. A. (2015). The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extreme physiology & medicine, 4, 16. https://doi.org/10.1186/s13728-015-0036-7
7. Arias-Fernández, P., Romero-Martin, M., Gómez-Salgado, J., & Fernández-García, D. (2018). Rehabilitation and early mobilization in the critical patient: systematic review. Journal of physical therapy science, 30(9), 1193–1201. https://doi.org/10.1589/jpts.30.1193
8. Hodgson, C. L., Schaller, S. J., Nydahl, P., Timenetsky, K. T., & Needham, D. M. (2021). Ten strategies to optimize early mobilization and rehabilitation in intensive care. Critical care (London, England), 25(1), 324. https://doi.org/10.1186/s13054-021-03741-z
9. Tipping, C.J., Harrold, M., Holland, A. et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med 43, 171–183 (2017). https://doi.org/10.1007/s00134-016-4612-0
10. Smith, Heidi A. B. MD, MSCI (Chair)1,2; et al. 2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility. Pediatric Critical Care Medicine 23(2):p e74-e110, February 2022. | DOI: 10.1097/PCC.0000000000002873
M0000018446 REV AA